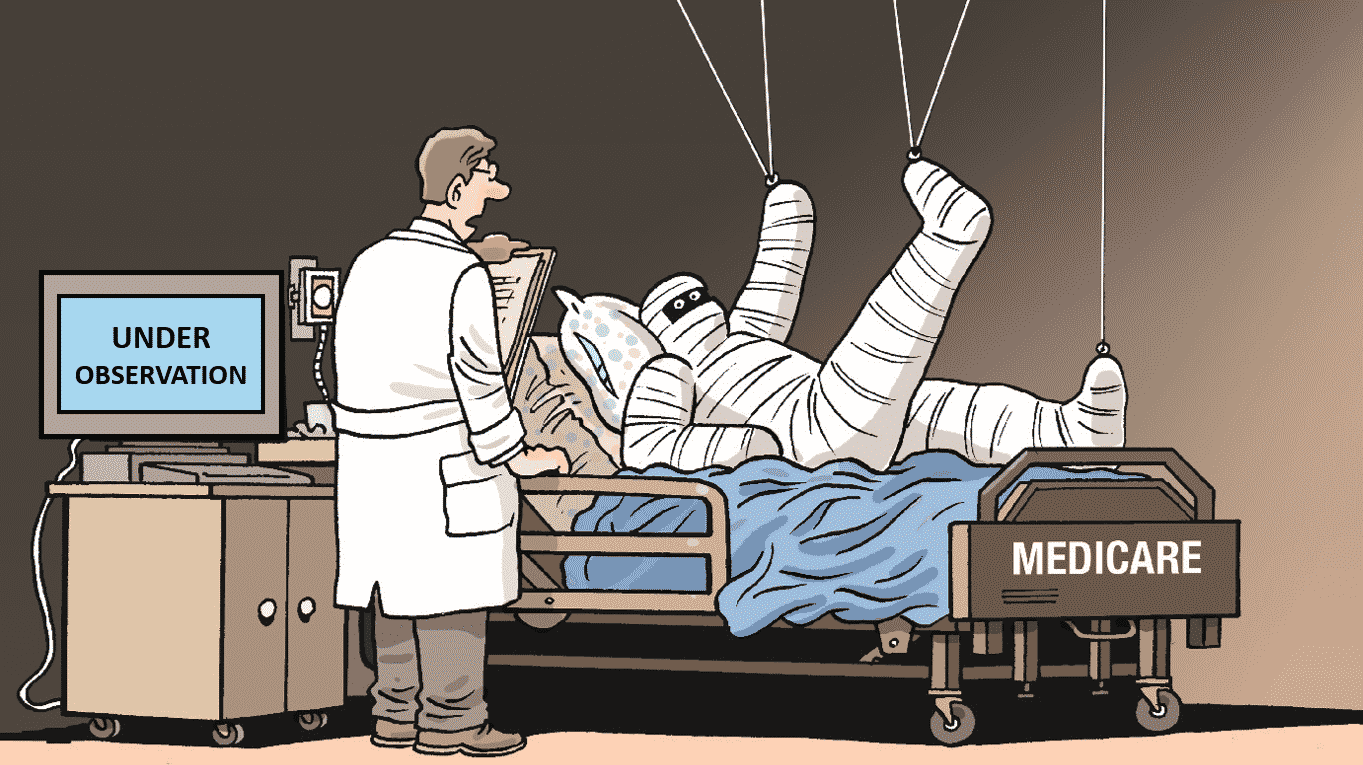
In an earlier blog, we explained the importance of understanding inpatient vs outpatient status with Medicare. The reason this is so important is because Medicare Part A only pays for skilled nursing services costs if you have been formally admitted to a hospital for 3 days as an inpatient – not if you were placed ‘under observation’ which technically means you have an outpatient status.
Over the last decade, the number of patients placed ‘under observation’ status at hospitals has increased dramatically. This is because if a hospital is audited by Medicare and they deem a patient should have been on ‘observation’ instead of admitted as an inpatient, Medicare can fine that hospital. As a result, hospitals are placing many people under observation because of the financial liability they face.
Remember that when someone is placed under observation, Medicare will not approve skilled nursing services to be covered. Meaning the patient will be responsible for 100% of those costs that would normally have fallen under Medicare Part A. This rule still applies even if you have a Medicare Supplement Plan F.
Moral of the story: make sure you are well informed on how Medicare covers services based on inpatient or outpatient status.
Have Questions? Contact us at (941) 405 – 3900.






One thought on “Two Words That Can Dramatically Affect Your Medicare Bill: ‘Under Observation’”